Wednesday, December 5, 2018
Monday, August 27, 2018
Rodger Kessler wins a ribbon!
Our own Rodger Kessler, PhD, Co-Principal Investigator, has once again been recognized for his extraordinary skills in Bonsai. This week at the Champlain Valley Exposition, Rodger received the Red Ribbon for his exquisite Colorado Blue Spruce (Picea pungens).
Congratulations, Rodger!
-Ben
Congratulations, Rodger!
-Ben
Monday, August 6, 2018
Introducing Alex Pond
Those of you who recently attended the IBHPC Annual Meeting have already met our newest staff member: Alex Pond has started as a Program Assistant in the UVM Department of Medicine where he will take responsibility for the CTS Graduate Program as well as helping out across all our activities. He did a great job last week supporting the meeting.
Alex was born and raised in Burlington, Vermont. He began his career at UVM working first at the Bailey/Howe Library and then Undergraduate Admissions before moving to Baltimore and joining the Graduate Admissions team at the Johns Hopkins School of Nursing. Following his time in Baltimore he lived in Santa Fe, New Mexico where he supported the CHRISTUS St. Vincent Family Medicine Residency program, whose mission was to train physicians in a community based setting serving the people of Northern New Mexico. He is very excited to return home and be joining the CTS/GIMR team at the College of Medicine.
Welcome, Alex!
- Ben Littenberg
Alex was born and raised in Burlington, Vermont. He began his career at UVM working first at the Bailey/Howe Library and then Undergraduate Admissions before moving to Baltimore and joining the Graduate Admissions team at the Johns Hopkins School of Nursing. Following his time in Baltimore he lived in Santa Fe, New Mexico where he supported the CHRISTUS St. Vincent Family Medicine Residency program, whose mission was to train physicians in a community based setting serving the people of Northern New Mexico. He is very excited to return home and be joining the CTS/GIMR team at the College of Medicine.
Welcome, Alex!
- Ben Littenberg
Saturday, August 4, 2018
Training to Deliver Integrated Care
Congratulations to CR Macchi and Rodger Kessler on the publication of Training to Deliver Integrated Care: Skills Aimed at the Future of Healthcare (Springer International Publishing AG)..
https://www.springer.com/us/book/9783319788487
This unique trainer’s resource offers a comprehensive blueprint for preparing clinicians for practice in the changing and challenging environment of integrated care. Based firmly in new evidence-based models of behavioral care in medicine, it sets out the aims and objectives of modern integrated care delivery in a streamlined pedagogy-to-practice framework. Teaching strategies for developing core skills and competencies, suitable across diverse educational and workforce development settings, are presented with data-based rationales and guidelines for design and implementation. Chapters also cover the range of essentials, from research support to business acumen to program evaluation methods, needed to meet bedrock goals of improved quality of care, clinical outcomes, and patient satisfaction.
The book’s comprehensive coverage:
- Reviews the evidence base for integrating medical and behavioral care.
- Provides empirically sound guidelines for training learners in integrated practice.
- Breaks down skill development into critical training objectives.
- Offers detailed content of a current degree program in integrative behavioral medicine.
- Recommends measures to support responsive, patient-centered, and sustainable training programs.
A robust guide to a more inclusive and effective future, Training to Deliver Integrated Care expands the healthcare horizon to accommodate trainers working in health psychology, general practice, primary care medicine, and consulting, as well as supervision and coaching professionals.
https://www.springer.com/us/book/9783319788487
Sunday, July 29, 2018
Welcome to our new Post-Doc - Lisa Watts Natkin
Lisa Watts Natkin, PhD is the IBH-PC project's new Post-Doctoral Research Fellow coordinating the collection, analysis, and management of qualitative data. She will help plan and conduct site visits and interviews, review project documents, code qualitative data, conduct thematic analyses, and support manuscript preparation. Recently, Lisa completed her PhD in Educational Leadership and Policy Studies at the University of Vermont (UVM). Her dissertation research explored student learning and teaching practices related to UVM’s new sustainability general education requirement. Findings are published in a peer-reviewed article. During her master’s degree, she helped to evaluate a program designed to motivate Brookfield Zoo members to participate in conservation behavior. The Teton Science Schools hired her to evaluate the effectiveness of their graduate program. During her doctoral program, Lisa evaluated the Sustainability Faculty Fellows (SFF) program, which seeks to develop a learning community among a multidisciplinary faculty cohort. Evaluation findings were published in two peer-reviewed journal articles. For the past two years, Lisa has been an evaluator working with Evergreen Evaluation & Consulting, Inc. She supported several U.S. Department of Education’s Office of Special Education Program grant funded programs. She assisted clients with instrumentation development, conducting interviews, collecting data, analyzing data, and writing reports. Lisa lives in Hinesburg with her husband, 3-year-old son, and dog.
We are really excited to have her on the team!
- Ben Littenberg
Sunday, July 15, 2018
New book by Roger Kathol
Roger Kathol, who is a leader in Integrated Behavioral Health with a special focus on Case Management (and a consultant to our project), has just released the second edition of The Integrated Case Management Manual. Published by Springer. Highly recommended.
-Ben Littenberg
-Ben Littenberg
Tuesday, July 10, 2018
New research om warm handoffs
Warm handoffs are often recommended as a great way to get patients who need Behavioral Health services from the Primary Care Provider to the Behavioral Health Provider. Not only are they in our IBH-PC toolkit, they are one of my favorite tools. They have great face validity, and in my experience, they work extremely well. So, I was quite surprised to see this recent report.
As the authors note, this is a retrospective analysis that is subject to unmeasured confounding, so a more complete story awaits an RCT. The article can be found online here.
- Ben Littenberg
Warm Handoffs and Attendance at Initial Integrated Behavioral Health Appointments
- Christine A. Pace, MD, MSc1⇑,
- Katherine Gergen-Barnett, MD2,
- Alysa Veidis, RN, MSN, NP-BC3,
- Joanna D’Afflitti, MD, MPH1,
- Jason Worcester, MD1,
- Pedro Fernandez, MD4 and
- Karen E. Lasser, MD, MPH1
+Author Affiliations
- 1Section of General Internal Medicine, Department of Medicine, Boston University School of Medicine and Boston Medical Center, Boston, Massachusetts
- 2Department of Family Medicine, Boston University School of Medicine and Boston Medical Center, Boston, Massachusetts
- 3Commonwealth Care Alliance, Boston, Massachusetts
- 4Department of Psychiatry, University of Texas Southwestern, Dallas, Texas
- CORRESPONDING AUTHOR: Christine Pace, MD, MSc, 801 Massachusetts Ave, 2nd Floor, Boston, MA 02117, Christine.pace@bmc.org
Abstract
Though integrated behavioral health programs often encourage primary care physicians to refer patients by means of a personal introduction (warm handoff), data are limited regarding the benefits of warm handoffs. We conducted a retrospective study of adult primary care patients referred to behavioral health clinicians in an urban, safety-net hospital to investigate the association between warm handoffs and attendance rates at subsequent initial behavioral health appointments. In multivariable analyses, patients referred via warm handoffs were not more likely to attend initial appointments (OR = 0.96; 95% CI, 0.79-1.18; P = .71). A prospective study is necessary to confirm the role of warm handoffs.
- Ben Littenberg
Wednesday, June 27, 2018
A unified model of Behavioral Health integration in Primary Care.
Congratulations to Mark McGovern and Kaitlin Dent from Stanford and Rodger Kessler from Arizona State on the publication of this commentary in Academic Psychiatry. They briefly and effectively lay out the argument for going beyond co-location by using team-based care and argue for a unified model including management of mood disorders, substance abuse and other behavioral issues in Primary Care. Good reading!
McGovern, M., Dent, K. & Kessler, R. A unified model of Behavioral Health integration in Primary Care. Acad Psychiatry (2018) 42: 265. https://doi.org/10.1007/s40596-018-0887-5 (paywall protected).
Sunday, June 17, 2018
Research synthesis on mental disorders and medical comorbidity
Many of you may have known about this report, but I just came across it while researching something else. It contains lots of background material in support of IBH-PC and related efforts. Very useful.
Druss BG, Walker ER. Mental disorders and medical comorbidity. Synth Proj Res Synth Rep. 2011;1-26. https://www.integration.samhsa.gov/workforce/mental_disorders_and_medical_comorbidity.pdf
This synthesis provides an overview of medical and mental comorbidity, with an eye towards current federal health reform efforts. It addresses the following questions: 1. What is the rate of comorbidity between medical and mental conditions and why is it so common? 2. What are the associated mortality, quality of care, and cost burdens of comorbidity? 3. What are the current evidence-based approaches for addressing comorbidity?
Druss BG, Walker ER. Mental disorders and medical comorbidity. Synth Proj Res Synth Rep. 2011;1-26. https://www.integration.samhsa.gov/workforce/mental_disorders_and_medical_comorbidity.pdf
This synthesis provides an overview of medical and mental comorbidity, with an eye towards current federal health reform efforts. It addresses the following questions: 1. What is the rate of comorbidity between medical and mental conditions and why is it so common? 2. What are the associated mortality, quality of care, and cost burdens of comorbidity? 3. What are the current evidence-based approaches for addressing comorbidity?
-Ben Littenberg
Tuesday, June 12, 2018
Poster by Kessler, Brenhoffer and van Eeghen: Frequently overlooked challenges of pragmatic trials
Rodger Kessler, Stephanie Brenhoffer, and Connie van Eeghen presented a poster at the Translational Science meetings in Washington in April.
Kessler RS, Brennhofer SA, van Eeghen C. Frequently overlooked challenges of pragmatic trials. Translational Science. Washington, DC. April 2018.
You can link to it here.
You can link to it here.
Friday, June 8, 2018
We are very excited to announce our clinics have recently received plaques noting their involvement in this research project! We are proud partners with all of our clinics and are grateful for their full participation in our research. These plaques will also serve to increase patient enrollment and patient knowledge regarding the study they are a member of.
A big thank you to Sylvie and Jessica for taking the initiative to highlight our partnership with our clinics and creating these plaques!
Wednesday, June 6, 2018
Association Between Social Determinants of Health and Physical Function in the IBHPC study
Here are preliminary results from the first ancillary study using data from IBH-PC.
Association Between Social Determinants of Health and
Perceived Physical Function in Adults with Comorbid Chronic Medical and
Behavioral Problems: A Cross-sectional Analysis
Kathleen Whitbread MD, Benjamin Littenberg MD
Background: Patients
with multiple chronic medical and behavioral health issues often perceive a
lower health-related quality of life, but little research explored the
association between socioeconomic factors and physical health. Social determinants of health (SDH) differ
from traditional socioeconomic factors by specifically addressing daily
challenges such as food, housing and income insecurity. We sought to describe
the association of SDH with physical function in a chronically ill primary care
population.
Methods: This is a cross-sectional
observational study of 154 randomly selected adults from the Integrating Behavioral Health and Primary
Care for Comorbid Behavioral and Medical Problems study. Subjects had at least one chronic
medical illness and one behavioral health need. An SDH score was calculated for
each subject based on 4 questions about their ability to meet their basic daily
needs including food, housing and other expenses. Physical function was
measured by the 12-item Duke Activity Status Index (DASI) which has been
validated against exercise testing with
measurement of peak oxygen uptake. Race was dichotomized as “White” vs. all others and Low Income was
defined as self-reported annual household income <$30,000. We used
nonparametric robust linear regression to assess the relationship between DASI,
SDH, and other social factors.
Results: Subjects
without any SDH challenges were found to have a mean DASI score of 31.4 METs
(95% confidence interval [28.3, 34.4]), compared to subjects identified as
having moderate (21.8 [16.0, 27.6]) or severe (19.1 [12.6, 25.7]), a
significant trend (P<0.001). Race
and low income were significantly associated with both SDH score and DASI and
were retained in multivariate linear regression to control for possible
confounding. Adjusting for race and low income reduces the strength of
association of SDH with DASI, rendering it non-significant, and demonstrating
confounding.
Conclusion: There
is an association between SDH and physical function in patients with chronic
medical conditions and behavioral health needs. However, other social variables
(e.g., income and race) confound the
relationship between DASI and SDH, making determination of the causal pathway
problematic. Does poor function lead to social challenges or vice versa? Unlike other socioeconomic variables,
however, housing and food insecurity can be directly addressed in the primary
care setting. Although there were
multiple limitations to this study including a small number of subjects and
lack of several predictors including age, this study suggests that such efforts
may be valuable. Social determinants of health are potentially modifiable risk
factors for poor physical function in the chronically ill.
________________________________________________________
Dr. Whitbread, an Internal Medicine Resident at the University of Vermont Medical Center, led the study and presented these preliminary results at Medical Grand Rounds in Burlington on May 25, 2018. As more baseline data come in, the analysis will be expanded and updated.
Thursday, May 24, 2018
Chronic care coordination by integrating care through a team-based, population-driven approach: a case study.
Here's a new article about one of the case studies that informed the IBHPC intervention. Congrats to Connie van Eeghen for this!
van Eeghen CO, Littenberg B, Kessler R. Chronic care coordination by integrating care through a team-based, population-driven approach: a case study. Translational Behavioral Medicine. 2018;8: 468-80. http://dx.doi.org/10.1093/tbm/ibx073
Patients with chronic conditions frequently experience behavioral comorbidities to which primary care cannot easily respond. This study observed a Vermont family medicine practice with integrated medical and behavioral health services that use a structured approach to implement a chronic care management system with Lean. The practice chose to pilot a population-based approach to improve outcomes for patients with poorly controlled Type 2 diabetes using a stepped-care model with an interprofessional team including a community health nurse. This case study observed the team’s use of Lean, with which it designed and piloted a clinical algorithm composed of patient self-assessment, endorsement of behavioral goals, shared documentation of goals and plans, and follow-up. The team redesigned workflows and measured reach (patients who engaged to the end of the pilot), outcomes (HbA1c results), and process (days between HbA1c tests). The researchers evaluated practice member self-reports about the use of Lean and facilitators and barriers to move from pilot to larger scale applications. Of 20 eligible patients recruited over 3 months, 10 agreed to participate and 9 engaged fully (45%); 106 patients were controls. Relative to controls, outcomes and process measures improved but lacked significance. Practice members identified barriers that prevented implementation of all changes needed but were in agreement that the pilot produced useful outcomes. A systematized, population-based, chronic care management service is feasible in a busy primary care practice. To test at scale, practice leadership will need to allocate staffing, invest in shared documentation, and standardize workflows to streamline office practice responsibilities.
van Eeghen CO, Littenberg B, Kessler R. Chronic care coordination by integrating care through a team-based, population-driven approach: a case study. Translational Behavioral Medicine. 2018;8: 468-80. http://dx.doi.org/10.1093/tbm/ibx073
Patients with chronic conditions frequently experience behavioral comorbidities to which primary care cannot easily respond. This study observed a Vermont family medicine practice with integrated medical and behavioral health services that use a structured approach to implement a chronic care management system with Lean. The practice chose to pilot a population-based approach to improve outcomes for patients with poorly controlled Type 2 diabetes using a stepped-care model with an interprofessional team including a community health nurse. This case study observed the team’s use of Lean, with which it designed and piloted a clinical algorithm composed of patient self-assessment, endorsement of behavioral goals, shared documentation of goals and plans, and follow-up. The team redesigned workflows and measured reach (patients who engaged to the end of the pilot), outcomes (HbA1c results), and process (days between HbA1c tests). The researchers evaluated practice member self-reports about the use of Lean and facilitators and barriers to move from pilot to larger scale applications. Of 20 eligible patients recruited over 3 months, 10 agreed to participate and 9 engaged fully (45%); 106 patients were controls. Relative to controls, outcomes and process measures improved but lacked significance. Practice members identified barriers that prevented implementation of all changes needed but were in agreement that the pilot produced useful outcomes. A systematized, population-based, chronic care management service is feasible in a busy primary care practice. To test at scale, practice leadership will need to allocate staffing, invest in shared documentation, and standardize workflows to streamline office practice responsibilities.
- Ben Littenberg
Sunday, May 13, 2018
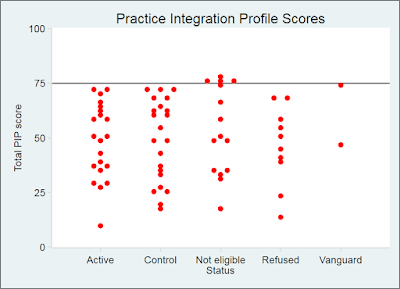
How well integrated are the participating practices?
Now that we have enrolled the sites, it's time to think about how well they are integrated. One way to look at that is the Practice Integration Profile. The PIP is a 30-item self-report measure that can be completed by providers, managers and staff at a primary care practice. It yields a score from 0 to 100 to indicate how well Behavioral Health is integrated into the practice in each of six domains: Workflow, Clinical Services, Provider Integration, Case Identification, Patient Engagement, and Workspace. There is also an overall or Total PIP score that is the average of the six domain scores. You can read more about the PIP and even try it out yourself at the PIP homepage.
To be eligible for the IBH-PC study, a practice needed to have a Total PIP score of no more than 75. This was to avoid recruiting practices that are already so well integrated that the IBH-PC redesign intervention just doesn't make sense. Why spend a lot of time and effort to integrate when you are already well-integrated?
Of the 118 practices we considered for the study, 70 provided at least 4 PIP surveys by various clinic staff. The Total PIP scores averaged 50 and ranged from 10 to 78. The 43 randomized clinics averaged 49 and ranged from 10 to 73. (The four practices with scores above 75 were ineligible.)
Happily, the stratified randomization worked as planned: the Active and Control groups are very similar in terms of both mean (48 vs. 49) and median (50 vs. 52), with P>0.9 by both Student's t and Wilcoxon rank-sum tests.
N.B.: Some of these PIPs were collected many months before the study actually began at the sites, so all randomized sites submit another wave of PIPs to be used as the baseline in the study analysis.
-Ben Littenberg
To be eligible for the IBH-PC study, a practice needed to have a Total PIP score of no more than 75. This was to avoid recruiting practices that are already so well integrated that the IBH-PC redesign intervention just doesn't make sense. Why spend a lot of time and effort to integrate when you are already well-integrated?
Of the 118 practices we considered for the study, 70 provided at least 4 PIP surveys by various clinic staff. The Total PIP scores averaged 50 and ranged from 10 to 78. The 43 randomized clinics averaged 49 and ranged from 10 to 73. (The four practices with scores above 75 were ineligible.)
Happily, the stratified randomization worked as planned: the Active and Control groups are very similar in terms of both mean (48 vs. 49) and median (50 vs. 52), with P>0.9 by both Student's t and Wilcoxon rank-sum tests.
N.B.: Some of these PIPs were collected many months before the study actually began at the sites, so all randomized sites submit another wave of PIPs to be used as the baseline in the study analysis.
-Ben Littenberg
Sunday, April 29, 2018
Study Progress
Now that site recruitment is closed, let's see what we have. There are 45 sites: 21 in the Active arm, 22 in the Control arm, and 2 Vanguard sites that are beta-testing parts of the intervention before we send it to the Active sites.
The sites are in 13 US states (Alaska, California, Georgia, Hawaii, Idaho, Kentucky, Massachusetts, New York, Ohio, Oregon, Texas, Vermont and Washington):
We'll have more details going forward, so stay tuned!
- Ben Littenberg
The sites are in 13 US states (Alaska, California, Georgia, Hawaii, Idaho, Kentucky, Massachusetts, New York, Ohio, Oregon, Texas, Vermont and Washington):
Here is a breakdown of the ownership of the 45 participating practices:
We'll have more details going forward, so stay tuned!
- Ben Littenberg
Monday, April 16, 2018
A Balanced Portfolio Model For Improving Health: Concept And Vermont’s Experience
Health Affairs recently published an article by James Hester (IBHPC Stakeholder Advisory Board member) about Vermont's efforts to rationalize health care delivery over the past decade or so. Jim had a front-row seat for much of this dramatic activity as a staffer for the state and later for CMS. It is well-written, engaging, and makes a compelling case for considering a holistic approach to social welfare as a vehicle for improving health and health care.
Hester J. A Balanced Portfolio Model For Improving Health: Concept And Vermont’s Experience. Health Affairs; April 2018. https://doi.org/10.1377/hlthaff.2017.1237
Hester J. A Balanced Portfolio Model For Improving Health: Concept And Vermont’s Experience. Health Affairs; April 2018. https://doi.org/10.1377/hlthaff.2017.1237
Abstract: A successful strategy for improving population health requires acting in several sectors by implementing a portfolio of interventions. The mix of interventions should be both tailored to meet the community’s needs and balanced in several dimensions—for example, time frame, level of risk, and target population. One obstacle is finding sustainable financing for both the interventions and the community infrastructure needed. This article first summarizes Vermont’s experience as a laboratory for health reform. It then presents a conceptual model for a community-based population health strategy, using a balanced portfolio and diversified funding approaches. The article then reviews Vermont’s population health initiative, including an example of a balanced portfolio and lessons learned from the state’s experience.
Great work, Jim!
- Ben Littenberg
Friday, April 13, 2018
Site Recruitment milestone
As of today, 43 clinics are enrolled in the IBH-PC study! This is a big milestone as our study design calls for 40 sites. (I'm juiced that we have a few extras - statistical power is a numbers game.) The randomization has yielded 21 Active practices and 22 in the Control arm. Baseline data collection has started and the data are starting to come in - very exciting!
Thank you to Juvena, Sylvie, Rodger and all the Cluster Leaders for making this happen.
-Ben Littenberg
Thank you to Juvena, Sylvie, Rodger and all the Cluster Leaders for making this happen.
-Ben Littenberg
Thursday, March 29, 2018
Update on the IBHPC
The first version of the IBHPC intervention is complete! It consists of:
- the online curriculum
- the toolkit, including
- team management suggestions
- a set of tactics for integrating behavioral and primary care
- step-by-step templates for clinic process redesign
- a guide for patient partners working on the redesign team at the clinics
- remote coaching for practice facilitators
The curriculum is a series of 15-30 minute multimedia modules in the Canvas learning management system and comes with continuing education credit. It is tailored for specific audiences based on their roles in the clinic: primary care providers, behavioral health providers, nurses, care managers, administrative staff, facilitators, managers and patient-partners. The workbook is available online as a PDF document than can be printed for local use. The remote coaching is delivered via phone and web by a team of experienced practice coaches from a secret location at IBHPC HQ.
This is a major milestone and I'm very grateful to the cast of thousands, led by Connie van Eeghen, Daniel Mullin, CR Macchi, Yuna Berman, Jen Lavoie, Paula Reynolds, Doug Pomeroy and Gail Rose.
For now, the intervention is the heart of our study. When the study is over (and we have some idea of how well it works!), we will make it available for use in a clinic near you...
- Ben Littenberg
Wednesday, March 28, 2018
IBHPC featured in webinar series on Health Systems Transformation
Betty Rambur, RN, PhD (Professor of Nursing at the University of Rhode Island and member of the IBHPC Stakeholder Advisory Group) is hosting a series of webinars on Health Systems Transformation with an emphasis on workforce development issues. The series started with a talk by Ben Littenberg, MD on Integrating Behavioral Health and Primary Care. It has been archived on line at https://web.uri.edu/ahc/2018/02/27/hstcwebinar1/
Future webinars are available free of charge. See https://web.uri.edu/ahc/hstc/
Future webinars are available free of charge. See https://web.uri.edu/ahc/hstc/
Thursday, March 15, 2018
Parinda Khatri on Barriers to Integrated Care
Parinda Khatri, MD, Chief Clinical Officer at Cherokee Health Systems and a member of our Stakeholder Advisory Group, was interviewed recently by NEJM Catalyst for their article on Care Redesign. Among the many insightful things she says is:
(Thanks to Jen Lavoie for sharing this link.)
- Ben Littenberg
"We used to go around the country and explain why integration is important — really having to explain the need. Everyone now knows why; they just want to know how.”Of course, that is the main reason we are doing the IBH-PC project - to sort out how best to achieve high-quality integration. Cherokee is an exemplar of excellent integration and has served as a model for our own efforts. It's good to see Parinda and company get the credit they deserve!
(Thanks to Jen Lavoie for sharing this link.)
- Ben Littenberg
Subscribe to:
Comments (Atom)